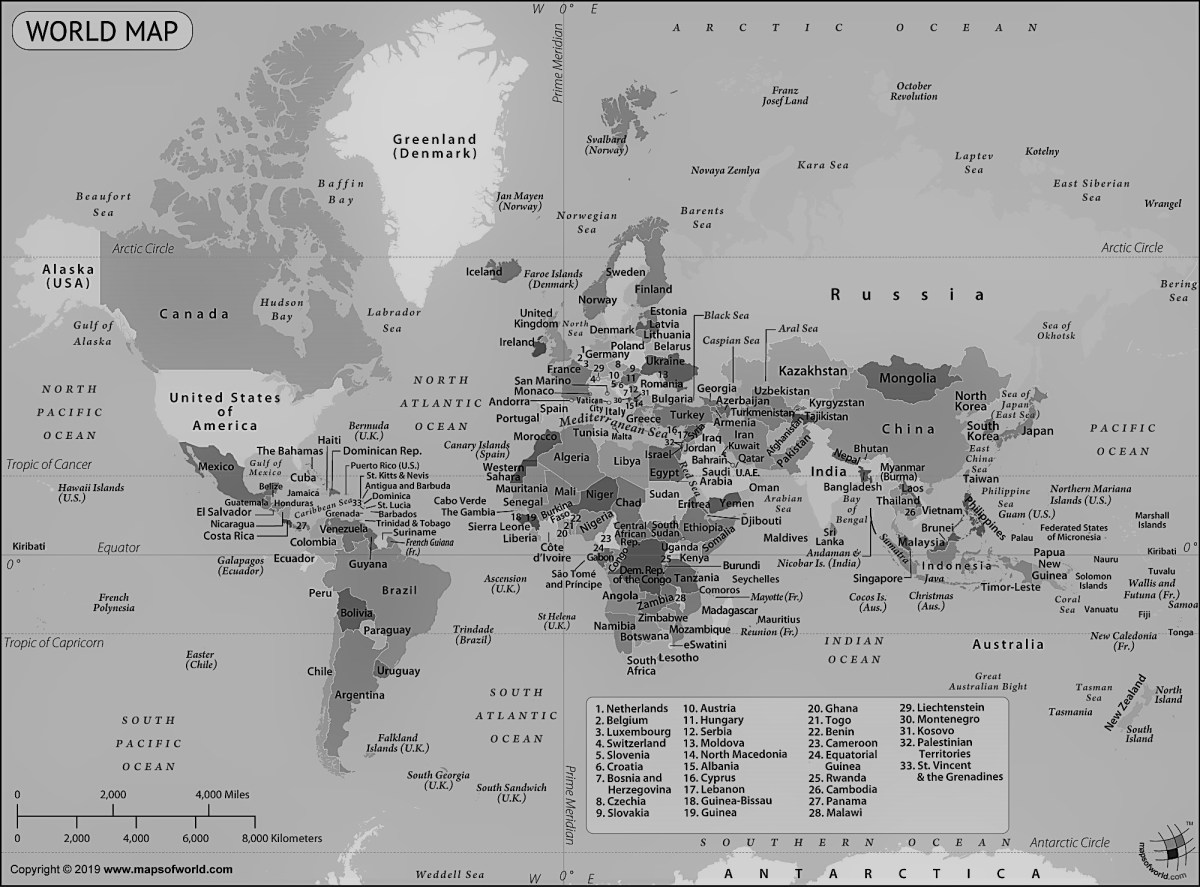
I met Andrew while on placement in Tonga last year and we’ve kept in touch. As of the 30th of May, the United Kingdom had 271,226 laboratory confirmed cases of COVID-19 and 38,161 deaths. I can’t begin to imagine how horrific this might be. We have been talking about how COVID-19 has impacted him as a medical student and I asked him to share his story:
“This is a crazy time, isn’t it? I turned 25 last month and had a big party planned for all of my uni mates, which would have coincided with our final day of placement. Sadly a higher power had other ideas.
“I’m a UK-based medical student who met Daisy and her friends while in Tonga last summer (or winter for the Australians/Kiwis reading this). I think it’ll be a while before I’m back down-under again.
“We first heard that there was a new disease in China around late-January. It wasn’t something that we thought much of at the time. My course-mates and I were too busy with placements and preparing for our finals; it seemed like a world away and something that shouldn’t concern us. “Stuff like this doesn’t affect England, it’ll never reach us poms.”
“Then in late February we began seeing the footage from Italy. Initially we were quite dismissive and we laughed at people rushing to go and stock up on toilet paper. An online video of two women fighting was circulating and while the hysteria was comical, it made light of what was going to develop into a serious situation. We just didn’t believe it and believed it was media hype trying to whip up a story.
“The severity and scale of the illness had probably been covered up by the Chinese media, but as more reports came out of Italy, we started to see how bad it was for the first time. We could see patients with severe respiratory distress in their hospitals, how the doctors were struggling to cope with the workload and how the streets were closed to prevent spread. “Oh dear – this is actually quite serious!” Perhaps the media hysteria had some substance to it, and it shouldn’t be disregarded so readily.
“Sporting events began to be cancelled, most notably the last weekend of the 6 Nations. Italy’s final games against Ireland and England were postponed at the request of the latter’s governments, and Ireland began to enforce social distancing within their country. But in spite of this, our borders to Europe were still open and one of the biggest horserace event of the year, the Cheltenham festival, had gone ahead with 250,000 spectators.
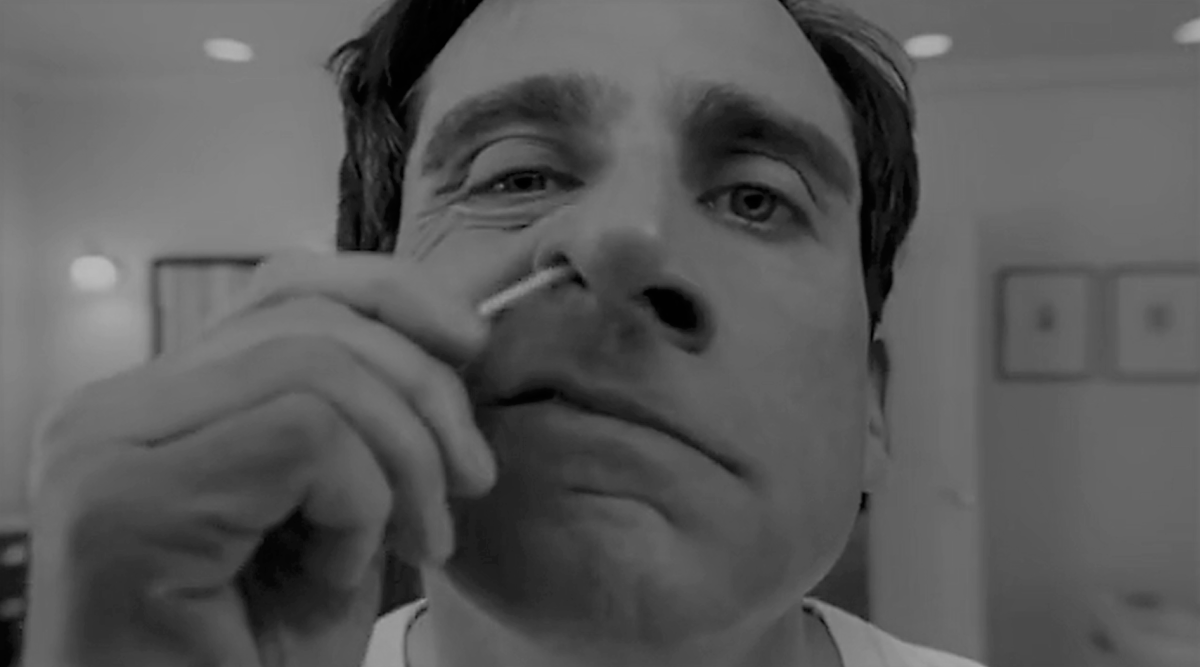
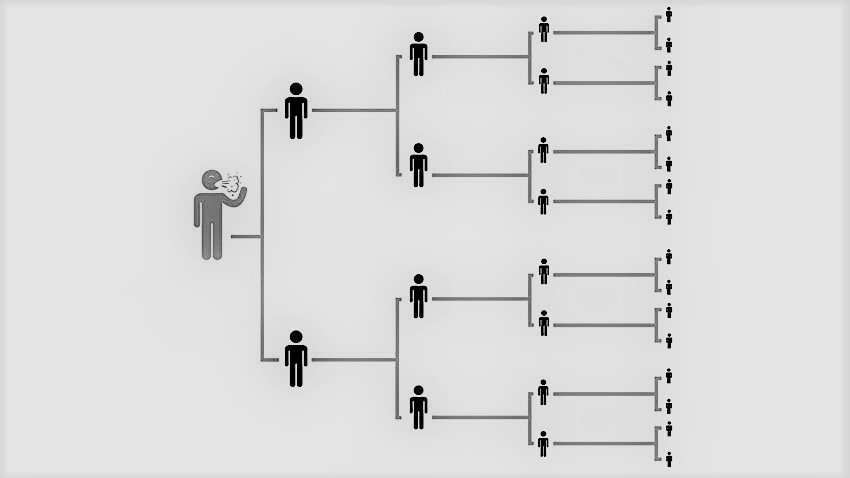
“At this point, I was on a respiratory ward, and very close to finishing. Most cases were in London with about a hundred deaths, and infections were beginning to pop up across the country. This was quite a scary time for my two placement buddies and I as we didn’t know when corona was going to reach Leeds on a large scale. Would we be seeing these patients, would we be able to finish our placement, would we be at risk of contracting the virus? The biggest worry was we could potentially spread it among the student population (in Leeds where I study, that’s 100,000 individuals) who would then spread it home to their families all over the country. We medical students would be an ideal vector.
“It seemed that our medical school thought this too. They told all students in the lower years to stop going to placement to minimise exposure, all teaching moved online to prevent the spread, and people were passed into the next academic year based on their placement reports and previous examination scores. I felt most sorry for the 4th years. While they have the toughest exams to sit (they dodged that bullet), this all meant their finals in year five would be much harder, and they missed out on their electives, the best holiday they would never have.
“Final years were told to keep going to placement. The General Medical Council declared final years were to be made a priority, so that we could qualify quickly and help ease the burden on the NHS. We were practically qualified at this point so were of some use on the wards. We would go and see patients before the consultants, prepare the notes and take the necessary bloods, helping to speed up the ward rounds. It was quite nice to feel as if we were of use.
“Then we started seeing infections in Leeds. When a student who was staying in halls [university accommodation] became infected, the entire university closed its doors, and every course moved to an e-learning platform. You couldn’t go to the libraries, the computer rooms or the on campus gym. In the evenings I’d come home from placement and see students filling their cars or getting picked up by their parents to go home for the inevitable lock-down. It felt like a scene from World War Z with all the cars parked outside and students abandoning their houses.
“Going back into the hospital after those first confirmed cases, the place had turned into a ghost town. Only patients who needed to be there were and on the floor was tape to encourage the two metre distancing. One of the respiratory wards was now exclusively for the COVID patients (along with ITU [intensive treatment unit]), no visitors were coming in and as many beds as possible had been emptied. It was strange being in the MAU [medical admission/assessment unit], which had been turned into the corona overflow unit, and there being no patients. All of these changes to prepare for the sudden spike had taken place in all of 48 hours.
“In spite of the apocalyptic tension, it was mostly business as usual. There was only one patient with a confirmed case and they’d been sectioned off. Staff were adhering to the new hygiene procedures and applying the necessary PPE [personal protective equipment], and it was all done with very little drama. Given what we were seeing in the news I was very surprised at how calm it all felt on the front line. I imagine as time has gone on and the number of cases have increased, this may have changed a bit.
“As previously mentioned, medical students are ideal vectors, and given we were on a respiratory placement, our consultants agreed to sign us off a week earlier than planned. It was a rather anticlimactic way to end six years of studying and placements. I’d imagined a big night out with my mates, and I’d even organised it, but our prime minister had closed all pubs and restaurants. It was completely the right decision by the government, but I hadn’t pictured medical school ending this way. Still, at least I got one for the gram…
“Then on the night of the 23rd, Boris Johnson gave his television address telling us that we must stay at home. I live with two other student doctors and I remember thinking, as we sat in one of our cluttered bedrooms watching, “This is what wartime Britain must have felt like.”
“When Boris had finished, we looked at each other and asked “What are we doing?” Do we stay in our small flat and only go out once a day, or do we pack our bags and go home to our families? We chose the latter, there was no way we were staying in our cramped flat in the middle of the city, where we’d only be allowed out once a day. If I was at home, I’d have my mother for company, a country park out the back of my house and a more comfortable area to live. Within an hour of Boris’ announcement, I had packed the essentials, and was gone.
“Settling into the new regime took a while. Day-to-day things like shopping, going to the gym, going for a walk and coming home from work had to be planned, as was choosing when and what to eat. My mother is a midwife, and as a frontline worker she was at a greater risk of contracting the virus, given she was meeting patients daily. Our front porch became an airlock; she’d come home, take off her uniform, take it through to the washing machine and go straight for a shower to wash off any virus particles before doing anything else. We came up with a meal plan involving foods with a long shelf life, and we batch cooked a lot of meals in the first week that I was home. If one of us became ill, at least we’d have an ample food supply and wouldn’t have to worry about cooking.
“This was made more difficult when the fridge suddenly broke. We couldn’t order a new one immediately as people’s panic buying had suddenly extended to second fridges, so we had to borrow a small one that a friend lent us, and when a new fridge did arrive, the deliverymen wouldn’t install it because of the risk of infection. Totally understandable, but my mother wouldn’t have been able to install it herself.
“The daily government reports added to the increased tension. We saw the figure of daily deaths rising and wondered if their measures were working. The media were reporting stories of a lack of ventilators, a lack of PPE, a lack of testing and an economic crisis for thousands of people. It was very much a picture of doom and gloom, which got a lot worse when Boris Johnson was taken to hospital after testing positive. The media’s portrayal of it all didn’t help with the country’s mood.
“You can only control the controllables however. So I got myself into a mental headspace where I would focus on the few things that I had some form of control over, mainly keeping the house tidy and revising for my exams, and would adapt to whatever was to come. We were told that we’d be doing an online assessment, and that our practical OSCEs [objective structured clinical examination] had been cancelled, so I spent most of my day knuckling down. Then about a week into lockdown, once we hit early April, the health secretary Matt Hancock announced that he was going to get final year medical students to start working early, to help on the front line. The medical school responded and told us that they were going to cancel exams, and pass people who met the list of criteria below:
- Passed fourth year the first time around
- Passed the National Prescribing Safety Assessment
- Passed all placements with no concerns
- Had signed off all skills
“I had met this criteria, but what did it mean? After over ten years hard work, was I finally a doctor? The confirmation email came through a few days later. “Dear Dr. Durham, congratulations on becoming a doctor!” Dear Dr. Durham? Bloody hell I’m going to have to get used to that.
“It was a bizarre way to finish medical school. Normally there’s a barbecue immediately after your final exam and you have a graduation ball when you’re done. It’s certainly not the ending that I’d imagined. The big positive of the current situation is that I don’t have to sit exams, and I can start earning some money straight away (which I’m very much looking forward to), and in the time it has taken to organise everything, it’ll be during the period after everything has peaked.
“What have I learned over the last 6 or so weeks in lockdown?
- I don’t trust the media. The majority of news these days is designed to be clickbait, to spark outrage and does little to really inform people in my humble opinion. It’s as if journalists have a hidden agenda that they are promoting; their careers, the political preferences. It makes for a very biased and uneven view, which doesn’t allow for intelligent discussion and at the time of an international crisis, undermining the government’s every decision in the hope of getting a reaction is dangerous and counter-productive.
- When there is a crisis, the British people come together. So many medical and healthcare students have volunteered to work as ward clerks, cleaners or doctors assistants in the hospitals near their medical schools (if they’re not in their final year). When the government asked for people to volunteers to deliver goods to the vulnerable 750,000 people stepped up. Captain Tom Moore (who celebrated his 100th birthday a few days ago), raised over £30 million for the NHS by doing 100 laps of his care home’s garden on a Zimmer frame, and every Thursday people have been clapping outside their front doors for all of the NHS workers.
- Society will be different for a long time. Until a vaccine is found and we know more about how this virus works, I think social distancing will be in place for a very long time.
“People who regularly go to the gym (like me) have had to adapt to exercising at home and make do with the equipment at hand. Who knew a bag of sand could be used for squatting and overhead pressing? I’ve become a lot fitter in this time.
“The way we connect to each other with Zoom and Facetime have been invaluable, and for the first time in a while I think that I’m better connected with my cousins than I have been for a long time.
“I’ve also broadened my culinary skills and value the outdoors a lot more than I previously used to.
“This is a very uncertain time for people, both with regards to their finances and their health but for me, there is a lot to look forward to. I’ve finished university and will be starting my first job as a doctor, financially I’ll have a lot more freedom and when this blows over, I can say that I was working at an incredibly testing time, and developed my clinical skillset.
“A positive mental attitude will be key going forward. Stay safe in the meantime.”
Thanks so much to Andrew for sharing your story! Andrew has a YouTube channel where he’s posted some videos of his travels: https://www.youtube.com/channel/UC1ZHHkYkDDiiRc-pF5AaqjQ, you might even find some video of the nursing girls and I swimming with the whales (thanks for preserving the memories Andrew)! Andrew talked about how the front of his house had become an ‘airlock’ for decontaminating before coming into the house. If you’d like to read up more on how I decontaminate coming home from work you can read about that here: https://daisyazmi.com/2020/04/17/cominghomefromworkdecontaminating/.
It’s been so interesting to hear about students from all over the world and catch up with friends. Next week’s post features Mahdid, a medical student in Newcastle and Angela, a recently graduated nursing student from Tonga!
For the WHO situation report where the statistics were gathered from please visit: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200530-covid-19-sitrep-131.pdf?sfvrsn=d31ba4b3_2
Subscribe for New Posts!